Patient-friendly guide from a clinical perspective, including when antibiotics are (and aren’t) appropriate, what to expect at the dentist and how to reduce your risk of ever needing a root canal.
Key Points
- A root canal (endodontic treatment) removes infected tissue (“pulp”) from inside the tooth, disinfects the canals, and seals them to save the tooth.
- It’s usually recommended for deep decay, cracks, or trauma that has reached the pulp and caused irreversible pulpitis or a dental abscess.
- Antibiotics alone don’t cure a dental abscess or replace dental treatment. They’re used only when there are signs of spreading infection or systemic illness, or when immediate drainage isn’t possible.
- The goal is source control: remove infection inside the tooth and prevent it from spreading or returning.
Do I need a root canal and why?
You may need a root canal when bacteria enters the pulp (through decay, a fracture, or a leaking filling) and the tissue becomes inflamed or infected.
Typical reasons your dentist recommends it include:
- Persistent toothache, especially on biting or with hot/cold.
- Prolonged sensitivity, swelling, tenderness to touch, or a gum boil (sinus tract).
- X-ray evidence of infection at the tip of the root (periapical radiolucency).
- A dental abscess arising from the tooth.
Left untreated, infection can cause worsening pain, facial swelling and, rarely, more serious complications.
Are antibiotics needed before a root canal?
Not routinely. UK guidance is clear: for most dental abscesses, local treatment (drainage, root canal, or extraction) is definitive.
Antibiotics are adjuncts reserved for:
- Spreading infection (cellulitis, lymph node involvement).
- Systemic features (fever, malaise) or high-risk patients (such as those who are immunocompromised).
- Situations where immediate operative care isn’t possible and temporary control is needed pending urgent dental treatment.
In the UK, antibiotics such as amoxicillin are prescription-only and should follow a clinician’s assessment. Responsible providers focus on a condition-led consultation and urgent dental treatment rather than “antibiotics first”.
What happens before a root canal?
- Assessment & X-rays: Your dentist examines the tooth, checks vitality, and takes an X-ray to plan treatment.
- Consent & plan: You’ll discuss options (root canal vs extraction), risks, benefits, costs, and the likely need for a crown on back teeth after treatment.
- Pain control: Local anaesthetic is used; you should feel pressure, not pain.
Step-by-step: What happens during a root canal
- Isolation: A rubber dam is placed to keep the area clean and protect your airway.
- Access: A small opening is made in the tooth to reach the canals.
- Cleaning & shaping: Infected pulp is removed and canals are disinfected with antibacterial solutions; files shape the canals for sealing.
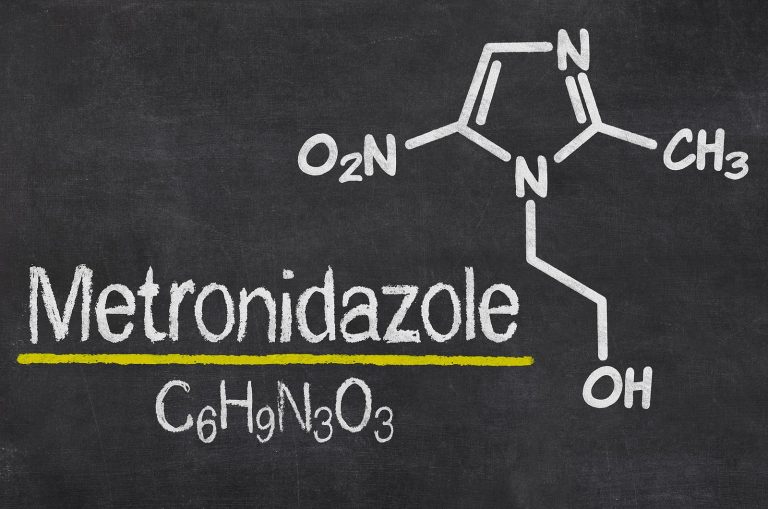
- Medication (if needed): Sometimes an antibacterial dressing is placed between visits.
- Sealing (obturation): Canals are sealed with a biocompatible material (e.g., gutta-percha) and the access is filled.
- Final restoration: A permanent filling or crown restores strength and seals the tooth against reinfection.
Appointments typically last 60–90 minutes; some cases need more than one visit (complex roots, large infections).
If you also have a dental abscess…
Your dentist will ensure drainage (through the tooth or via a small gum incision if needed). This relieves pressure and helps infection resolve. Antibiotics are added only when indicated (see above).
Recovery and aftercare following a root canal
- Pain relief: Discomfort usually improves within 24–48 hours; take simple analgesia (e.g., paracetamol/ibuprofen if suitable for you) as advised.
- Diet & hygiene: Soft foods for 1–2 days; brush as normal, keep the area clean.
- Protect the tooth: Avoid hard biting until the final crown is fitted (back teeth are prone to fracture without a crown).
- When to call back: If pain/swelling worsens, you develop fever, or the temporary filling comes out.
Risks, success rates, and alternatives to root canals
- High success rate when canals are thoroughly cleaned and the tooth is well restored.
- Possible risks: persistent infection requiring re-treatment, fracture if not crowned, or (less commonly) extraction if the tooth can’t be saved.
- Alternative: Extraction ends infection faster but leaves a gap; you may later consider an implant/bridge.
How to prevent root canals
- Brush twice daily with fluoride toothpaste (spit, don’t rinse).
- Clean between teeth (floss or interdental brushes).
- Limit free sugars, especially between meals and before bed.
- Regular check-ups with your dentist/hygienist to spot and treat decay early.
- Don’t ignore cracked fillings or tooth injuries and seek prompt care.
Urgent “red flags”: seek same-day help (A&E/urgent dental)
- Swelling under the tongue/floor of mouth, trouble swallowing or breathing, and trismus (can’t open mouth).
- High fever, rigors, confusion, rapidly spreading facial swelling.
- You feel very unwell or are immunocompromised.
Author: Dr Javeria Kiran Ahmed
Credentials: Dental Surgeon (GDC No. 244004), Qualified from University of Bristol 2013, BDS. Specialist Interest: Restorative Dentistry, Occlusion, Treatment of Complex Dental Cases, Facial Aesthetics, and Clear Braces